
For decades, mainstream cardiology has reduced atherosclerosis to a cholesterol problem. The solution offered is simple: lower LDL with statins, thin the blood, and operate when necessary. And that is why modern cardiology is a complete failure. Their story and practice of medicine are both incomplete and dangerous. Atherosclerosis is not only about fats; it is about oxygen starvation, acidic microenvironments, and microbial infiltration — especially fungi. To treat the arteries as mere clogged pipes is to overlook the complex ecology of disease that occurs within them. Atherosclerosis isn’t merely clogged arteries—it is arteries starved of oxygen, invaded by fungi, and acidified by the environment.
Atherosclerosis is generally described as an inflammatory and degenerative disease of the arteries, involving:
- Endothelial damage (the inner lining of blood vessels)
- Oxidized LDL cholesterol deposits in arterial walls
- Immune response & chronic inflammation
- Plaque formation that narrows and stiffens arteries
However, in recent decades, researchers have discovered infectious footprints within arterial plaques — bacteria, viruses, and, in particular, fungi. Several studies have identified fungal DNA and antigens inside atherosclerotic plaques. Common culprits:
- Candida albicans (the most common human fungal pathogen)
- Aspergillus species
- Cryptococcus
Chronic Low-Grade Infection
- Fungal organisms can persist in the bloodstream at very low levels.
- They trigger immune activation and chronic inflammation, which are key to the development of atherosclerosis.
- Molecular Mimicry
- Fungal cell wall components (like β-glucans and mannans) can confuse the immune system, leading to auto-inflammatory reactions against blood vessels.
- Endothelial Dysfunction
- Fungi can damage or adhere to endothelial cells, making the vascular lining more permeable to cholesterol and toxins.
- Pro-Coagulant Effects
- Fungal infections are associated with increased platelet aggregation and clotting, which accelerates plaque instability.
Hypoxia: The Suffocation of Arteries
This is the final chapter I am adding to the second edition of the above book.
In all severe disease states, we find a concomitant low oxygen state.
Low oxygen in the body tissues is a sure indicator of disease.
Hypoxia, or lack of oxygen in the tissues, is the
fundamental cause for all degenerative diseases.
Dr. Stephen Levine – Molecular Biologist
Healthy arteries are alive and require oxygen, which is delivered through the tiny vasa vasorum. When plaques thicken the arterial walls, this hinders the oxygen supply. Starved tissues suffocate. Hypoxia, a condition characterized by low oxygen levels, is not a passive bystander. It drives cardiovascular disease:
- Inflammation ignites – Oxygen deprivation activates HIF-1α, a hypoxia-inducible factor that switches on inflammatory and atherogenic genes (Semenza 2014; Akhtar et al. 2015).
- Cholesterol sticks – Hypoxia promotes uptake of oxidized LDL, fueling foam cell formation (Feng et al. 2017).
- Plaques destabilize – Hypoxic tissue releases VEGF, prompting the formation of fragile new blood vessels that rupture within plaques (Sluimer et al. 2008).
The cycle is vicious: Plaque → hypoxia → more plaque → more hypoxia. Oxygen, Hydrogen, and CO2 restore life to suffocating tissues.
CO2 is the most powerful way to release armies of
oxygen into the cells. It is CO2 that liberates
oxygen for healing. It is CO2 that makes oxygen safe.
If you want to live forever, know that enduring youth can be yours with enough oxygen. Dr. Arthur C. Guyton says, “All chronic pain, suffering, and diseases are caused by a lack of oxygen at the cell level.” Insufficient oxygen means insufficient biological energy, resulting in anything from mild fatigue to life-threatening disease. “Oxygen plays a pivotal role in the proper functioning of the immune system,” said Dr. Parris M. Kidd. Low oxygen conditions lead directly to inflammation. Chronic inflammation mirrors our body’s state of low oxygen.
And the key to oxygen is carbon dioxide. When we are deficient in CO2, we suffer from hypoxia. Under clinical conditions, low oxygen and low carbon dioxide generally occur together. Therapeutic increase of carbon dioxide, achieved by inhaling this gas diluted in air, is often an effective means of enhancing blood and tissue oxygenation.
As physiological studies have shown, hypocapnia constricts blood vessels, resulting in decreased perfusion of all vital organs. In emergencies, when these conditions are extreme, the organs and tissues of the body are not receiving an adequate blood flow.
The Dana-Faber Cancer Institute says, “Normal human cells need just the right amount of oxygen — not too much nor too little — to survive and stay healthy. This critical balance is regulated by an intricate oxygen-sensing process in the body,” the discovery of which earned the 2019 Nobel Prize in Medicine shared by Dana-Farber scientist William G. Kaelin, Jr., MD, and two other researchers. “This mechanism enables people to adapt to living at high altitudes and bring more oxygen to cells during exercise.” It also allows for healthy arterial walls.
Acid Conditions: Fertile Soil for Disease
When oxygen is in short supply, cells switch to anaerobic glycolysis. The byproduct is lactic acid, which pools inside plaques and lowers local pH. The direct effect of oxygen on pH in water is negligible, comparable to temperature variations; however, the indirect effects are significant. Without sufficient oxygen levels, cells cannot detoxify themselves, and acids accumulate. Without enough oxygen, cells turn cancerous, die, or indeed suffer from inflammation.
Acidification intensifies disease:
- Endothelial injury – Acid pH directly damages the vessel lining (Chesler et al. 2004).
- Inflammation – Acidosis activates macrophages and enzymes that erode plaque stability (Tang et al. 2013).
- Thrombosis – Acid promotes platelet aggregation, thereby increasing the risk of clot formation (Engelmann & Massberg, 2013).
Acid conditions trap oxygen, inflame vessels, and turn plaques unstable. And acid provides the perfect soil for fungal growth.
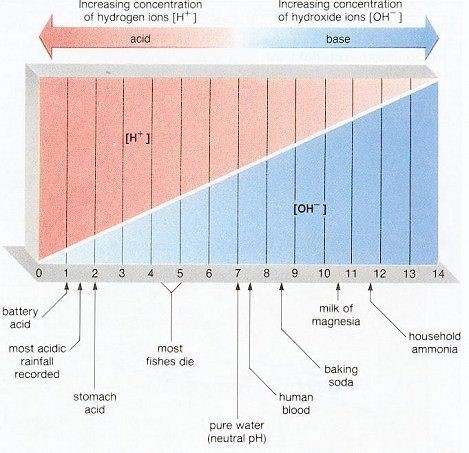
Being acidic means two things. First, it means low oxygen conditions; second, it means low voltage or energy conditions, because, in physics, we know that pH is a measure of voltage. If one does not understand pH medicine, then one cannot fully comprehend the physiology of oxygen and its significance in the treatment of vascular and other diseases.
Fungi: The Hidden Accomplice in Atherosclerosis
Multiple lines of evidence confirm fungi in plaques:
- Fungal DNA was identified in 26.8% of human atherosclerotic plaques (Candida albicans, C. guilliermondii) (Masoumi et al. 2015).
- Molecular analyses detected fungal rDNA in coronary plaques (Ott et al. 2007).
- Animal models: systemic Candida infection accelerates atherosclerosis (Yoshikawa et al. 2011).
- At the cellular level, Candida promotes the formation of foam cells and the release of inflammatory cytokines (Zhu et al., 2021).
Mechanisms of damage:
- Fungal toxins damage the endothelium (Calderone & Fonzi, 2001).
- Biofilms shield fungi from immunity (Chandra et al. 2001).
- Platelet aggregation and clotting are triggered (Kondori et al. 2011).
- Acid pH drives Candida from yeast form to invasive hyphae (Sudbery 2011).
Hypoxia and acid create the habitat; fungi exploit it.
Bicarbonate: The Forgotten Antifungal
Here lies the overlooked remedy: sodium bicarbonate. Unlike statins, bicarbonate works at the root of the ecological issue in blood vessels. Sodium bicarbonate effectively reduces inflammation caused by increased blood acidity.
- Neutralizes acidity – Fungi thrive in acid; bicarbonate restores alkalinity (Jensen et al. 2013).
- Blocks virulence – Bicarbonate inhibits Candida’s switch to invasive hyphae (Davis et al. 2000).
- Weakens biofilms – Sodium bicarbonate destabilizes fungal biofilms (Kim et al. 2018).
- Improves oxygenation – Buffers acidosis, enhancing oxygen release via the Bohr effect (Liu & O’Rourke 2013).
In vitro studies have shown that sodium bicarbonate at concentrations of 1–5% significantly inhibits Candida growth (Magalhães et al., 2009). Bicarbonate disarms fungi not by killing them, but by changing their environment.
Terrain-Centered Therapy
If atherosclerosis is an ecological disease — hypoxia + acidosis + fungi — therapy must restore the terrain:
- Oxygen therapies (EWOT, hyperbaric oxygen) – Reverse suffocation (Thom 2011).
- Bicarbonate – Neutralizes acid, suppresses fungi, improves oxygen delivery.
- Hydrogen therapy – Protects mitochondria from oxidative damage (Ohsawa et al. 2007).
- Magnesium – Dilates vessels, stabilizes heart rhythms, and supports mitochondrial energy (Altura & Altura 1995).
CO2 Inhalation Therapy – Dilates the blood vessels.
Together, these form a new model of cardiology: not cholesterol management, but terrain restoration. Cholesterol management is achieved through the use of PPC (polyenylphosphatidylcholine) and cyclodextrins.
Conclusion: Breathing Life Back Into the Arteries
Atherosclerosis is not simply clogged arteries. It is:
- Starved arteries (hypoxia)
- Acidified arteries (acidosis)
- Infected arteries (fungi)
Mainstream cardiology treats the symptoms with drugs and interventions, but ignores the ecology of cardiovascular disease. By restoring oxygen, neutralizing acidity, and suppressing fungal growth, we move toward an actual cure, as long as cyclodextrins are used in conjunction with PPC and other essential medicines employed in my Natural Cardiology approach.
Where there is oxygen, there is life.
Where there is alkalinity, fungi fail.
Where there is balance, the heart endures.
Atherosclerosis is a condition characterized by the accumulation of plaque in the arteries. The cure begins with breathing life back into them — remembering that sometimes the most potent medicine is the simplest: bicarbonate restoring balance against the fungi of death.
Dr.Sircus is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Subscribe now





comments