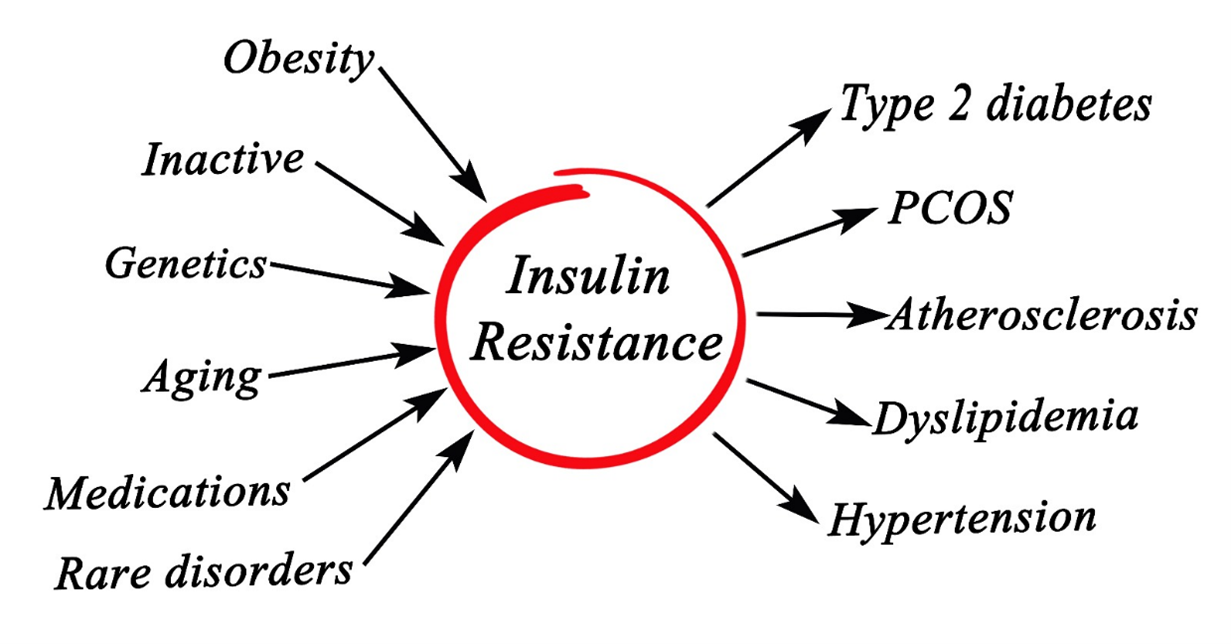
One of the significant threats to global health in the 21st century is insulin resistance, which is the key factor in the development of type 2 diabetes, cardiovascular disease, fatty liver disease, neurogenerative disease, and obesity-associated cancers. Understanding the molecular basis for insulin resistance leads to specific therapy that helps prevent this common disorder, and we now have a medicine that cleans up the mess in the vascular system after years and even decades of our bodies’ being under the sway of insulin resistance.
Insulin resistance (IR) is associated with an impaired biological response to insulin stimulation of key target tissues, particularly liver, muscle, and adipose tissue. IR impacts glucose utilization, resulting in a compensatory increase in beta-cell insulin production and hyperinsulinemia.
The hormone insulin, produced by the pancreas, regulates blood glucose, or sugar from our food, by allowing it to enter the body’s cells, which are used for energy. Insulin resistance—found in lean and overweight individuals—occurs when the body’s cells don’t effectively respond to insulin and take in glucose, leading to high blood sugar levels. Insulin resistance (IR) is the subnormal response to insulin action on target tissues. Studies suggest that IR increases the risk of hypertension.
Dr. Benjamin Bikman says, “We know that insulin resistance is at the core of most chronic diseases that are killing us. Insulin is a hormone that literally affects every cell of the body. But if those cells become insulin-resistant, you start to spread disease. 88 % of adults in the United States have some insulin resistance.” He also says, “Stress hormones will create insulin resistance pretty quickly. Sleep disturbances as well, and, of course, inflammation will cause insulin resistance. Few understand that high levels of insulin will also cause insulin resistance.”
Low serum and intracellular magnesium concentrations are associated with insulin resistance, impaired glucose tolerance, and decreased insulin secretion. Magnesium improves insulin sensitivity, thus lowering insulin resistance. Magnesium and insulin need each other.
What causes high insulin levels that will create insulin resistance? Stress, insomnia, and inflammation can be fast causes of insulin resistance and can often be resolved quickly. But the slow, insidious cause is overeating, especially if on a high-carbohydrate diet, which most people are. In conjunction with eating too many times a day, this does not allow insulin levels to drop. The cells get tired of all the insulin and start resisting. Eating too much and too frequently is deadly in the end. With so many overweight and obese people, we can see why health is in the trash for so many Americans.
Dr. Luc Tappy says, “The equivalent of the fructose in 8-10 cans of
Coke or Pepsi a day—is a pretty high dose, leaving people to become
insulin-resistant, and triglyceride increases in just a few days.[i]”
The term insulin resistance encompasses a broad continuum, ranging from individuals who maintain normal glucose homeostasis due to increased endogenous insulin production and do not yet have diabetes to individuals with diabetes who require exogenous insulin to maintain glucose homeostasis. Insulin, especially at high concentrations, can accelerate the atherosclerotic process by multiple mechanisms, including increased LDL synthesis/secretion, vascular smooth muscle cell growth and proliferation, activation of genes involved in inflammation, increased collagen synthesis, and enhanced LDL cholesterol transport into arterial smooth muscle cells.[ii]
Dr. Ron Rosedale says, “Insulin floating around in the blood causes plaque build-up. They didn’t know why until recently, but Insulin causes endothelial proliferation. Every step of the way, Insulin causes cardiovascular disease. It fills the body with plaque. It constricts the arteries. It stimulates the sympathetic nervous system, increasing platelet adhesiveness and coagulability of the blood.”
The heart suffers from dangerous nutritional deficiencies,
including a lack of sun and Vitamin D, magnesium, and iodine.
Multiple studies have demonstrated that insulin resistance strongly predicts atherosclerotic cardiovascular (CV) disease. Insulin resistance is associated with atherosclerosis, meaning Hyperinsulinemia accelerates the development of atherosclerosis. Insulin resistance raises blood sugar levels, and high blood sugar leads to inflammation, which damages the lining inside arteries. The suggestion that insulin is associated with atherosclerosis is based on clinical, epidemiologic, and experimental evidence. Coronary, cerebral, and peripheral artery atherosclerosis is associated with abnormally high insulin responses to oral glucose. Dr. Elliott Joslin noted that insulin has necessary indirect actions on the vascular system through its regulation of lipids and the development of hardening of the arteries.
Atherosclerosis, the underlying cause of heart disease and other vascular disorders, is characterized by endothelial dysfunction and a limited capacity to produce nitric oxide. It is a vicious cycle. Diseased arteries cannot generate enough protective nitric oxide, and low nitric oxide levels set the stage for further damage, hypertension, and increased risk of cardiac events.
This explains why nitroglycerin is such an effective therapy for angina. It triggers nitric oxide production, which dilates narrowed coronary arteries, improving circulation and delivering much-needed oxygen to the heart muscle.
Metabolic syndrome can also be known as insulin resistance syndrome (IRS) because the underlying insulin resistance is the etiologic factor responsible for developing cardiometabolic disturbances. Insulin resistance characterizes type 2 diabetes and metabolic syndrome, disorders associated with an increased risk of death due to macrovascular disease.
According to a 2024 national survey, 70% of Americans are unaware of peripheral artery disease (PAD) – the most common vascular disease in which leg arteries become narrowed, reducing or cutting off blood flow, contributing to 400 amputations performed each day in the United States. This all starts with insulin resistance.
Many people with blocked arteries or atherosclerosis are unaware that they have it until they develop symptoms such as angina or claudication. Claudication is a medical term usually referring to impairment in walking or pain, discomfort, numbness, or tiredness in the legs that occurs during walking or standing and is relieved by rest. Unfortunately, the first time that someone realizes that they have atherosclerosis is only when they have an event such as a stroke or a heart attack.
Cardiovascular disease is a leading cause of morbidity and mortality worldwide and significantly affects the quality of life of hundreds of millions of people. Atherosclerosis causes 4 of 10 deaths, with drug treatment limited to incremental advances in lipoprotein management. Modern medicine is not particularly savvy when it comes to arterial disease.
High glucose levels are dangerous for the arteries. Roughly one in four Americans with diabetes is unaware that they have the disease. Thus, untreated diabetes increases glucose, or sugar, in the blood, damaging the inner linings of both big and small arteries. The arteries respond by layering on plaque, a substance that fills the arteries so that oxygen-rich blood has difficulty getting through to the eyes, kidneys, legs, and feet. Sugar is an arterial poison. So is stress.
Treating the Long-term Effects of Insulin Resistance
Now comes the recent discovery of a new wonder drug that safely strips cholesterol out of vascular plaque. This means we now have access to cyclodextrins, the Ultimate Vascular Medicine, which are safer and more effective than statin drugs. Instead of using statins to control cholesterol levels chemically, with side effects including increased incidence of diabetes and cancer, with cyclodextrins, we reduce obstructions all over the vascular system and even beyond into the organs. Cyclodextrins administered intravenously or rectally are the way to reverse decades of plaque buildup quickly.
Recent research suggests Cyclodextrins may play a role in metabolic disorders, including insulin resistance, by influencing cholesterol metabolism, lipid accumulation, and inflammation—all of which are key factors in insulin resistance and type 2 diabetes. Cyclodextrins promise to improve insulin sensitivity by reducing cholesterol buildup, inflammation, and lipid accumulation. Thus, Type 2 Diabetics should use cyclodextrins to improve glucose control in insulin-resistant individuals.
How Cyclodextrins May Affect Insulin Resistance
-
Cholesterol and Lipid Metabolism
- Insulin resistance is strongly linked to lipid accumulation and cholesterol imbalances, particularly in the liver and muscle.
- HPβCD (2-hydroxypropyl-β-cyclodextrin) has been shown to enhance cholesterol efflux from cells, preventing lipid buildup that impairs insulin signaling.
- Studies in obese and diabetic mice have shown that HPβCD reduces liver fat accumulation, improving insulin sensitivity.
- Reduction of Inflammation
- Chronic low-grade inflammation is a major driver of insulin resistance.
- Cyclodextrins, particularly HPβCD, have been found to reduce pro-inflammatory cytokines (TNF-α, IL-6), leading to improved insulin signaling.
- By clearing cholesterol from macrophages (immune cells), cyclodextrins may help prevent the inflammatory response that disrupts glucose metabolism.
- Fatty Acid and Adipose Tissue Regulation
- Insulin resistance is linked to excessive visceral fat and dysregulated fatty acid metabolism.
- Some studies indicate that cyclodextrins may help modulate adipocyte (fat cell) function, preventing lipid-induced insulin resistance.
- By reducing ectopic fat deposition in skeletal muscle and liver, CDs may help restore normal insulin function.
Treating The Main Cause of Insulin Resistance
Magnesium participates directly in glucose metabolism disorders in humans.[iii] There is an essential connection between insulin resistance and magnesium. The incidence of insulin resistance and metabolic syndrome correlates with magnesium (Mg) availability.[iv] Magnesium is a vital mineral involved in over 300 enzymatic reactions, including those regulating glucose metabolism and insulin sensitivity. Research suggests that low magnesium levels are associated with an increased risk of insulin resistance, type 2 diabetes, and metabolic syndrome.
Below is just a summary. Much of Natural Cardiology is dedicated to magnesium for treating cardiovascular disease. It is an essential medicine (not just a supplement) that needs to be first in every treatment protocol. If one wants to avoid a stroke or cardiac arrest, it is best to take these words seriously, or your family might find you one day suddenly dead or incapacitated with a stroke. The strangest aspect of modern medicine and its hordes of doctors is that they continue to ignore magnesium to the detriment of all their patients. If Kennedy wants to see a revival of American health, he should start a national magnesium program. Magnesium deficiency is the most basic epidemic in America.
How Magnesium Influences Insulin Sensitivity
- Enhances Insulin Action
- Magnesium is necessary for insulin receptor function. Without enough magnesium, insulin cannot effectively bind to its receptors, leading to insulin resistance.
- Regulates Blood Sugar Levels
- Magnesium helps transport glucose into cells, which are used for energy. Low magnesium levels impair this process, contributing to higher blood sugar levels.
- Reduces Inflammation
- Chronic inflammation is a key driver of insulin resistance. Magnesium has anti-inflammatory properties, helping to lower markers like C-reactive protein (CRP).
- Lowers Oxidative Stress
- Magnesium acts as an antioxidant, protecting cells from oxidative stress, which is known to impair insulin signaling.
- Supports Mitochondrial Function
- Mitochondria, the energy powerhouses of cells, require magnesium for ATP production. Healthy mitochondria improve glucose utilization and metabolic function.
Magnesium Deficiency and Insulin Resistance
- Studies have shown that people with type 2 diabetes and metabolic syndrome often have lower levels of magnesium.
- Deficiency can be caused by:
- Poor diet (low intake of magnesium-rich foods)
- High sugar consumption (which increases magnesium excretion)
- Chronic stress (which depletes magnesium)
- Certain medications (e.g., diuretics, proton pump inhibitors)
- Digestive disorders (like Crohn’s disease, which impairs absorption)
Throughout Natural Cardiology, you will find information on magnesium. It is the ultimate heart medicine, while cyclodextrins are the ultimate vascular medicine. Combined, they hold the potential to vanquish much of the death and suffering of heart and vascular disease.
[i] “Toxic” effects of sugar: should we be afraid of fructose?
Luc Tappy; BMC Biology 2012, 10:42 http://www.biomedcentral.com/1741-7007/10/42
[ii] Insulin Resistance and Atherosclerosis: Implications for Insulin-Sensitizing Agents
Antonino Di Pino, Ralph A DeFronzo. Endocrine Reviews, Volume 40, Issue 6, December 2019, Pages 1447–1467, https://doi.org/10.1210/er.2018-00141
[iii] Nutrition Volume 38, June 2017, Pages 54-60. Effect of magnesium supplementation on insulin resistance in humans: A systematic review
[iv] Diabetes Obes Metab. 2011 Mar;13(3):281-4. Oral magnesium supplementation reduces insulin resistance in non-diabetic subjects – a double-blind, placebo-controlled, randomized trial
Dr.Sircus is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Subscribe now




comments